This video was part of a roundtable discussion involving surgeons Christina Y. Weng, MD, MBA; John B. Miller, MD; Raymond Iezzi Jr, MD; and Suzie A. Gasparian, MD. An edited transcript of the case presentation and discussion follows below:
Raymond Iezzi Jr, MD: I’d really like to thank everybody for the opportunity to be here and present. This is a really interesting case. It's a technique that was sort of a MacGyver move to figure out how to get an IOFB out of the eye. This is a gentleman who was hammering metal and had a metallic foreign body enter his eye through his pars plana. The patient is phakic and has really good vision. It’s a technique that I had used a long, long time ago and the video got deleted—I'm talking like 6 years ago—it was a gentleman that was walking through a field, and somebody shot a shotgun, and one of the pellets from the shotgun entered his eye. It was very large—looked like a musket ball because it was so big—and it was very, very heavy. I used this technique to encircle this sphere, which I couldn’t grab with forceps because it was just physically too large. I was really surprised that this technique encircled the sphere and was firmly holding it. I could even shake the instrument, and the sphere, when I got it out of the eye, would not come off of the instrument.
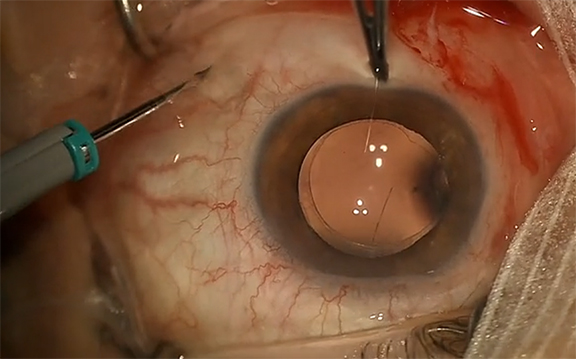
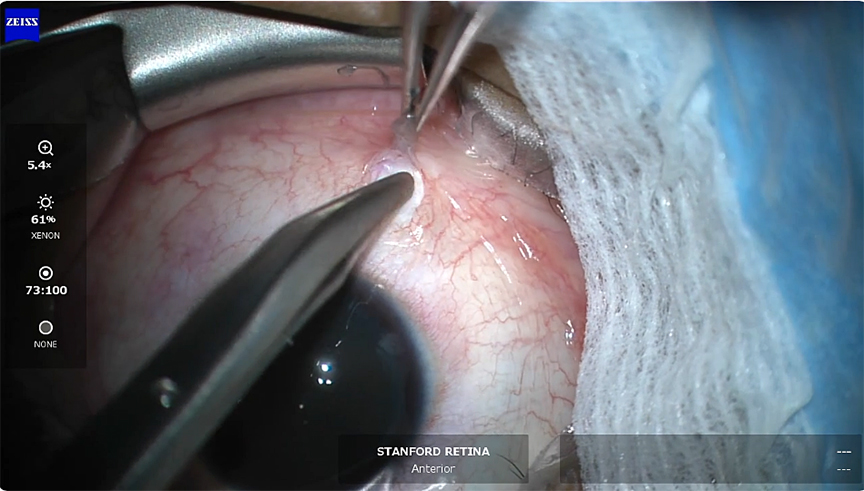
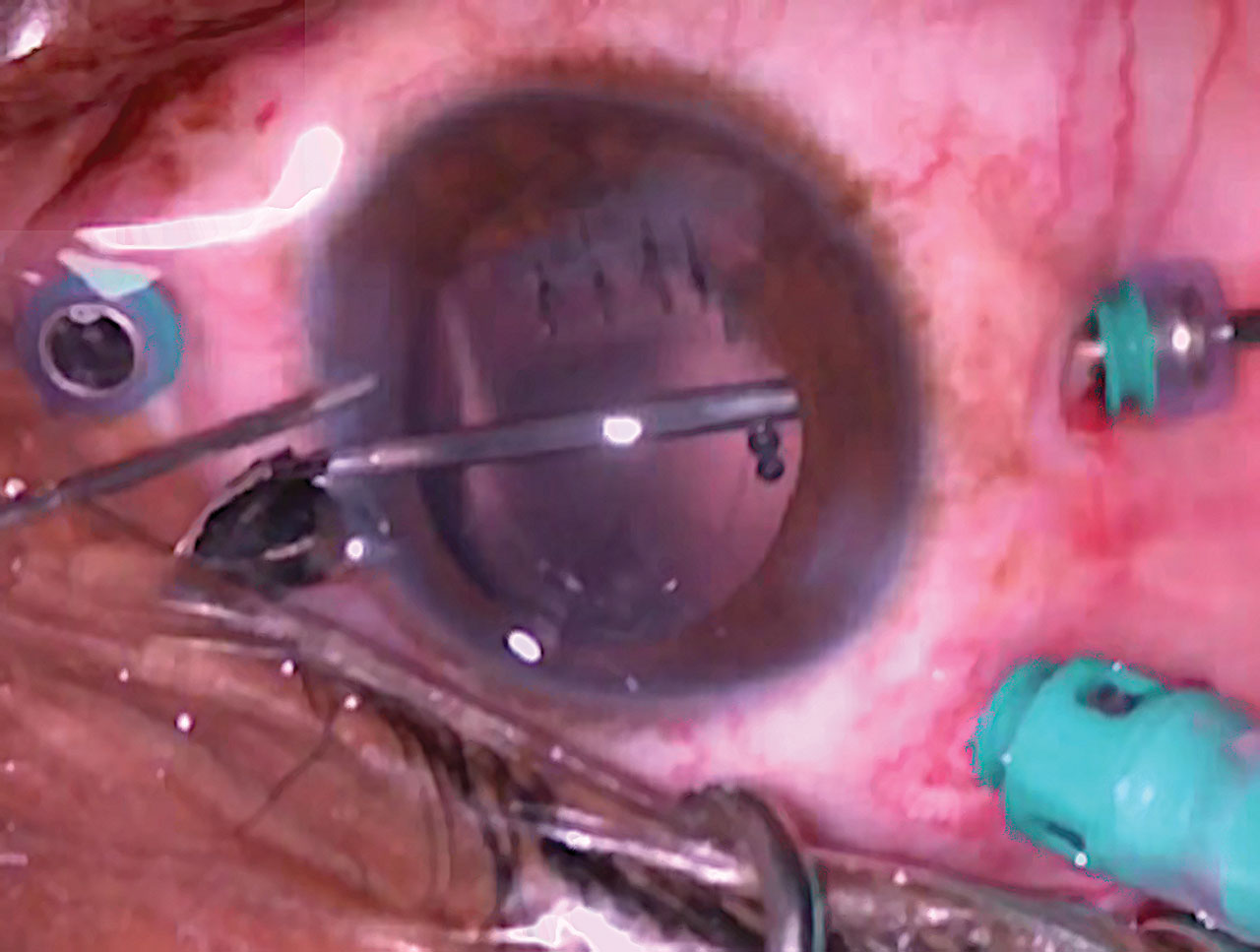
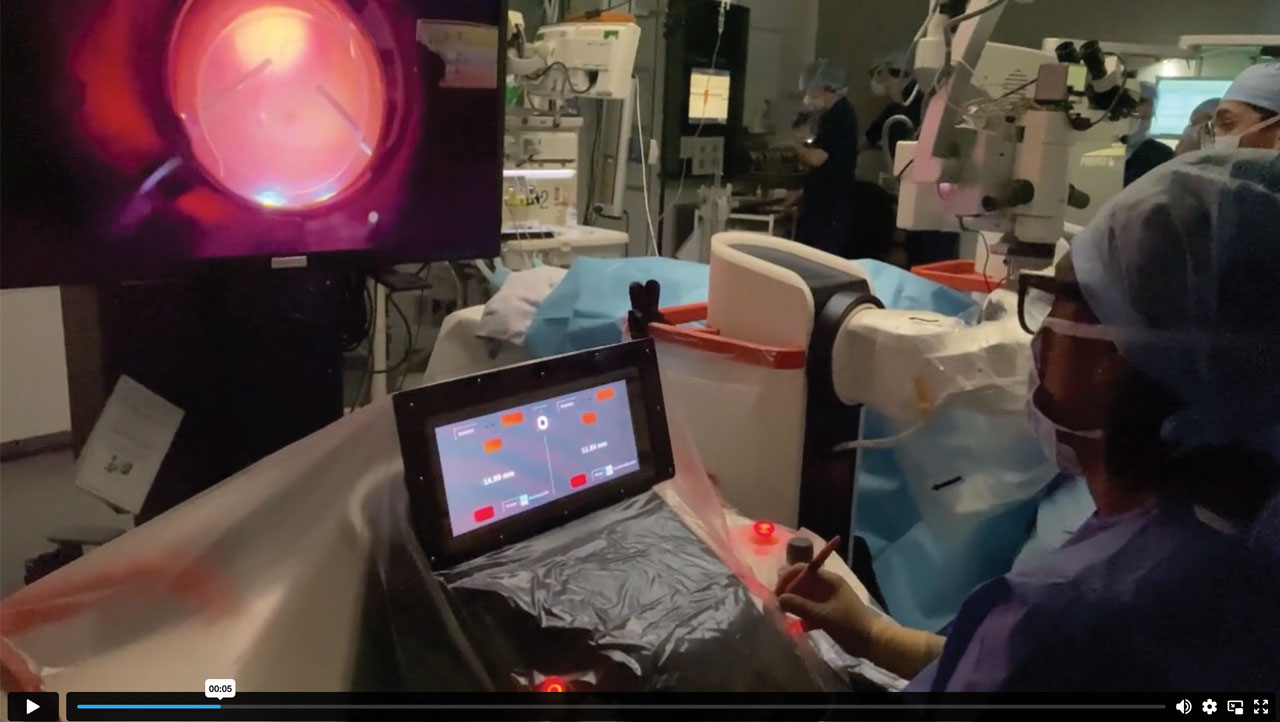
I want to show everybody how I make this. This is an intraocular snare. Basically, I start with—in this case, it was a 23-gauge cannula, but you could do it with a 25-gauge cannula. This is a 23-gauge straight cannula and a 5-0 nylon suture. I’m going to play the video, where basically I'm just threading the 5-0 nylon right into the lumen of the 23-gauge straight cannula, and we just create a loop. I cut the needles of this off, and we just use the suture portion of it. When it's through well enough, I grab both ends and I pull it along and make my loop. We’re basically creating our own loop. Then all you need is a Q-tip, and you just push that into the hub of the cannula. So with 3 items that we pretty much should all have in our operating room almost anywhere, we should be able to make this loop. Getting it into the valved cannula is a little bit of a trick. I use a light pipe or forceps to get it in through the valve and then feed it in this way.
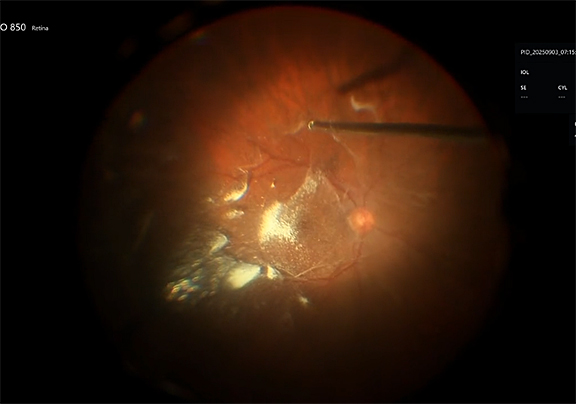
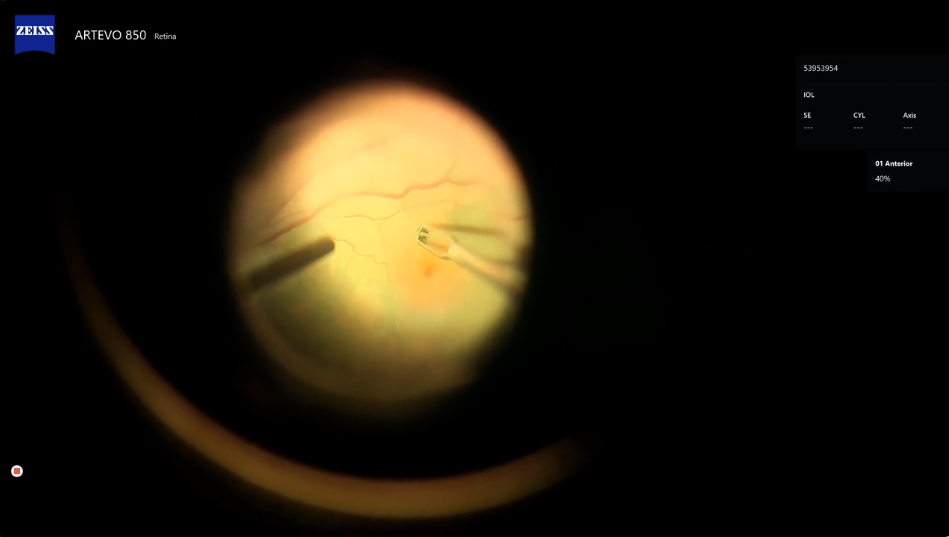
The reason why I like this technique is because it allows us to work with the intraocular foreign body in a closed system, so I don't have leakage from a large sclerotomy. I can adjust the size of the loop according to what I'm going to grab and this actually acts as an instrument. I can physically manipulate the foreign body in position. Now my fellow is depressing, and here I am nudging around it. My fellow is going to pull on the strings for me, and now I’ve grasped it. One of the keys is, as you’re pulling up on the string, that the surgeon has to advance the metal cannula toward the foreign body. Otherwise, it'll just kind of fall off, so you have to advance the instrument toward the foreign body as your assistant pulls up on the 2 strings. And then, this is where you open the eye. I could have diathermized to make this look prettier for the video, but I was just interested in getting it out. So there, we’re done. That’s all there is to it.
At the present time, I’ve done 5 cases, if you include that large heavy metal ball from the shotgun. I’ve also taken out glass and some metal that was embedded. You could actually use the loop to physically manipulate the foreign body, get it at the right angle. The other thing that's really interesting is that it will hold on to very complex shapes. It's sort of as if the nylon physically molds to the foreign body and just simply doesn’t let go.
I’ve found this to be very useful and I really enjoyed the last case. One time I had an IOL back there and both haptics came out sequentially and I literally had an optic laying on the back of the retina. The iris was stuck to the host of a corneal transplant and there was a tube, a Seton tube with a plate, so I didn't have an anterior segment and I couldn't make a scleral tunnel to get it out. So I actually took it out like an IOFB using this technique, where I lassoed the optic with no haptics and I took it out through the sclera. So that’s the case.
Dr. Weng: That is so incredibly genius, Ray. These types of cases tend to come in the middle of the night and there is nothing more frustrating than trying to find your pair of IOFB forceps with a staff that does not know where your instruments are, etc., so I love how this is sort of a makeshift pair of IOFB forceps. You mentioned that you had tried it on a shotgun bullet—is that similar to a heavy BB pellet? Would it work for a very spherical object?
Dr. Iezzi: Perfectly spherical, super heavy, laying down there. It’s like pushing a medicine ball around. I was able to engage it and it wouldn’t come off. I could get it out the same way I got this one out. At the end I was hovering over the cornea and I was shaking it back and forth and it wasn’t coming off. So you get this perspective that somehow the nylon sort of permanently molds to the foreign body.
Dr. Weng: That's amazing. One other point I want to make is that I like that you’re externalizing through the same sclerotomy through which your cannula was placed. That’s just pure elegance.
Dr. Iezzi: One little trick associated with that is as opposed to making our sclerotomy radial, it's actually better if you make it parallel to the limbus so that you can extend the same linear wound. Otherwise, you get a T incision. This was the first case I had done subsequent to the one I had done 7 years ago and I didn't do that, so I had a little T at the end of my sclerotomy that I had to add a couple of extra stitches for. To be really slick, you want to make your sclerotomy parallel to the limbus.
Dr. Miller: This is a beautiful case and a great technique, and thank you for teaching us again as usual. [You’re] always a wizard of new and novel ideas and very practical mechanical thinking, thank you. I was curious how the nylon interacts with a non-vitrectomized eye or more specifically a non-vitrectomized area of the posterior segment where the IOFB is. Sometimes these BBs or musket balls or different things are embedded in thick vitreous. For that reason I have often used a magnet, because the force is pulling it away from the vitreous. What is your experience with the nylon in a case like that? What have you seen?
Dr. Iezzi: That’s a great question. In this particular case, the IOFB hit the juxtafoveal region. It didn't hit the fovea. This gentleman wound up 20/20 and retained his lens. It bounced off of the fovea, as they often do, and it wound up in the vitreous base. When we've vitrectomized, we took the vitreous skirt but it was still encumbered in the vitreous base down there. When I used the loop, I nudged the foreign body out of the V base. So it was working in the quagmire of the vitreous base. We were able to encircle it and then pull it away and we didn’t create a break or anything. I don't know what it would be like to use this in a completely non-vitrectomized eye. It’s conceivable that with the foreign body we might be bringing vitreous along with the loop. Probably I’d want to have some vitrectomy going on there.
Dr. Miller: I think once you snared it, you basically could then try to vitrectomize if you had a chandelier in here. My fear would be doing too much vitrectomy to get at the foreign body and then subsequently dropping it again onto the macular surface.
Dr. Iezzi: Good point. I have to say, during the retrieval of this one, I could see it coming out of the V base pretty quickly. Too bad you didn’t have the audio of me saying, “Pull…Pull!” [Laughs.] You know, rapidly pull the string. I didn’t want it to fall down, so your point is really well made.
Dr. Weng: Another great learning point, John, that you reminded me of is that IOFBs love to hide in the vitreous base and you want to avoid the temptation of going right after them before your vitrectomy is completed which is a rookie mistake. You really just want to focus on the vitreous and get as much of it out as possible. If you can freely mobilize that IOFB, that’s even better. Because the last thing you want to do, as you said, is to tug at the vitreous surrounding IOFB and create some sort of iatrogenic nightmare that you have to clean up later on. These patients are already susceptible, as we know, to having retinal detachments down the line.
I wanted to ask, Ray: you said this one had missed the lens and the lens was not violated. [Dr. Iezzi: Yes.] Unfortunately, a lot of patients with trauma and IOFBs aren't quite as lucky. One of the big debates that we always have at my institution is whether the lens is taken at the time of IOFB removal or if it’s left. Do you guys have strong thoughts about which approach you prefer?
Dr. Iezzi: I personally would take the lens immediately, only because I don't want to add any sort of anaphylactic reaction. I don’t want uveitis superimposed on a healing open globe. So that lens is gone, I don’t even think twice. We have ways—Suzie showed a wonderful method for getting a lens in. I'd say, get the lens out, get your work done, close the eye, go home, and refer it to your favorite anterior seg doc to go back and do a modified Yamane.
Dr. Weng: I feel the exact same way. John, do you have any different thoughts?
Dr. Miller: Ray, you showed a case where you didn’t need to take the lens because it wasn't violated, but I agree that most of them there's either a clear violation, inflammation, or suspicion of a lens issue. If there’s any question, I take the lens. I like to do a scleral tunnel, because I didn’t have Ray’s technique, but the scleral tunnel basically allows you to have a very stable wound that you can directly visualize the removal of the foreign body out if the lens is gone. It’s a very nice technique and you can sometimes even sit the IOFB in front of the iris, just like Suzie showed on her IOL case. You have more structures, you’ve got better visualization. I always am a little nervous in that few seconds where the IOFB is passing under the dilated pupil and you don't know what's happening—is it going to come out through your sclerotomy or not. This case looks great—you got a snare, it's a different situation—but you never know if it's going to fall off the forceps if you’re coming out through the pars plana.
Dr. Gasparian: If there is any question while preoperatively examining the patient about lens capsule violation, even any cortical material coming forward into the anterior chamber, that’s just a ticking time bomb. In the operating room, the view is going to go bad really quickly, so I think the easiest thing to do is just remove the lens. We can always put a lens in later. So not only when it comes to impeding the view but also dealing with the post-operative inflammation induced by lens particles, in an already hot, angry eye, I'll take the lens, especially if there’s any risk that it’s going to impede the view to do my retina work. Beautifully done case. It makes me think that this is a self-made flex loop, basically, and so I expect to see this in the form of a flex loop in the future to aid in our IOFB removals.
Dr. Iezzi: I have actually used the finesse loop to take out Yutiq implants when the IOP went crazy, so these loops have utility. The benefit of this one is we can make it quite large if we need to. It’s adjustable.
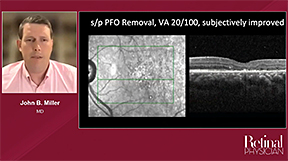
Dr. Miller: One other teaching point before we wrap the case is that these do have a very high rate of retinal detachment. We did a large case series [and found] about 50% of these develop retinal detachment. I teach and really push for everyone to try to pull up PVD as much as possible, to get rid of as much vitreous as you can, before or after you take the IOFB out. I would not leave the hyaloid down if you have a reasonable view. Try to pull a PVD and take the extra time because it's going to be a PVR machine if you have even a strike site, somewhere, it's going to proliferate and contract and you then have a very bad PVR detachment to deal with later with hyaloid down.
Dr. Weng: Truer words have never been said, John, and I never really breathe easily until several months down the line because that’s exactly what you're watching for even if they look beautiful upon closure. To that point, does anyone add prophylactic laser in these types of cases, aside from the impact point of course?
Dr. Iezzi: I’m so glad you asked that question. I think the impact itself is all the destruction needed to get the chorioretinal scar so I don't add laser, especially in the macula region, unless there's an RD that I have to repair. I think the impact itself is all you need.
Dr. Miller: I think you’re asking about extended vitreous base laser. I don't usually do that. If you're thinking about prophylactics of detachment, just blanket laser 360, I don't do. I do apply laser to the strike site, but maybe Ray’s point is correct, I don't have to. I do also diathermze, and occasionally cut in a very neat way, a tiny little red otomy around it because you will find that the edges of the retina already has folds and signs of contraction so you really want to try to release that while you're in there if you can. I would apply laser to that as if it was a drainage retinotomy.
Dr. Weng: It's a great point, John. You almost see it exerting traction on the strike site so I love that point that you made.
Dr. Iezzi: When I trained, we were taught exactly that—where you would do a retinectomy, like a very fine linear cut of the retina, because the presumption was that vitreous had incarcerated from the impact into the retina perhaps into the choroid and sclera. I think the key is to make sure that the hyaloid is up. I do use triamcinolone (Triesence; Harrow) in all of these cases to assure that we don't have residual hyaloid, because I think that's ultimately why we see recurrence of PVR. A point very well made, John. I’ve come away from cutting retina, but in favor of labeling the vitreous using triamcinolone and making sure it's up and there’s no remnants in that site because as you know this this is a PVR machine, as you said.
Dr. Gasparian: I agree with all the points you all are making. I always put dilute Kenalog-40 [Bristol Myers Squibb] down just to make sure again we've induced a full PVD. Same with patients who've had retained cataract lens fragments post–cataract surgery, we work on removing the vitreous first and then remove the foreign body or lens fragments themselves so as not to cause more vitreoretinal traction and have the risk of breaks there. So same with these cases, remove all the vitreous and then go after the foreign body. I would have a lower threshold to laser around the impact site. But I also don't do 360 laser in these cases.
Dr. Weng: Fabulous points. Thanks again for sharing that case, Ray, that was really genius. RP