In late November, the Centers for Medicare and Medicaid Services (CMS) released its final 2026 rule for hospital outpatient departments (HOPDs) and ambulatory surgery centers (ASCs), setting a 3.3% overall increase to payment rates under the Outpatient Prospective Payment System (OPPS). The final rule maintains CMS’s use of Ambulatory Payment Classifications (APCs) to reimburse groups of similar procedures, with intraocular procedures grouped into 6 levels (APC 5491 to APC 5496).
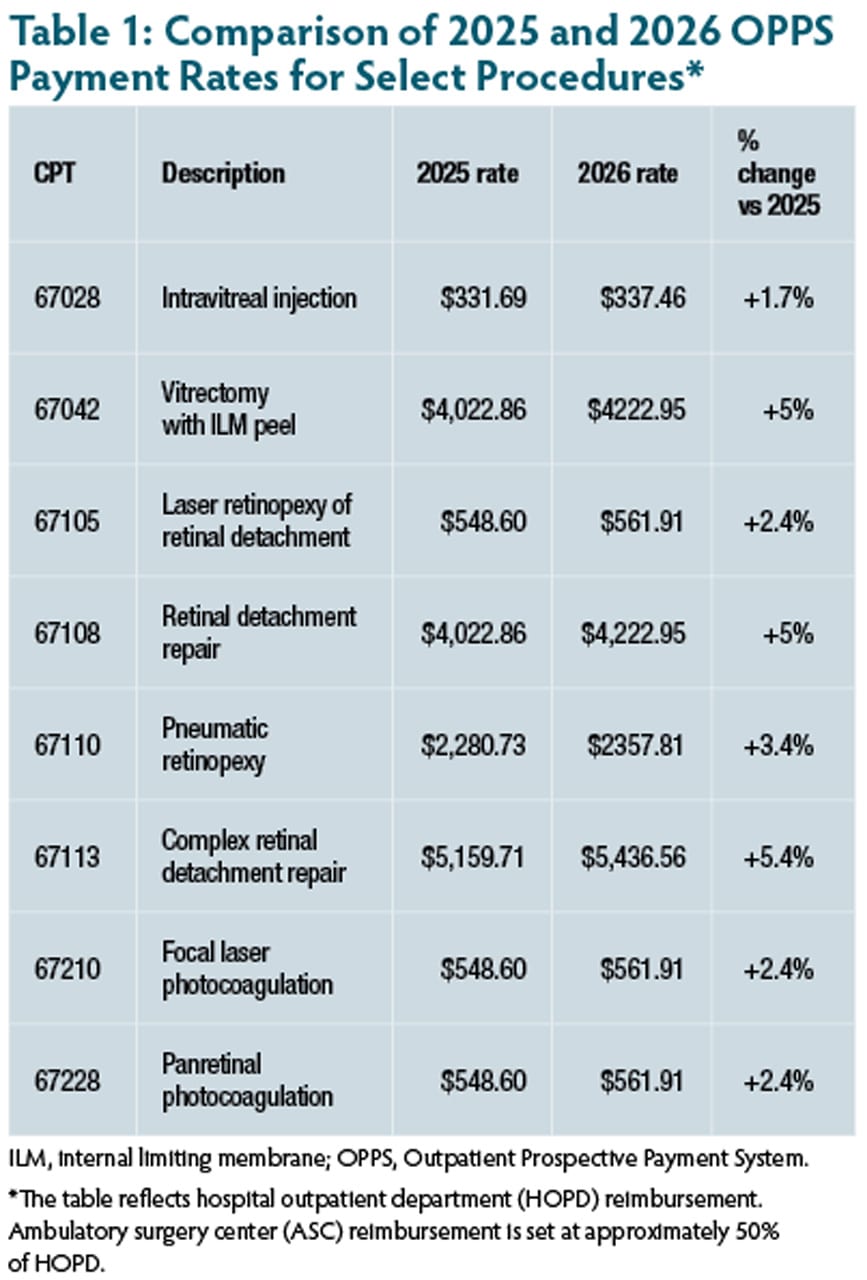
Intraocular level 2 (APC 5492), which includes lower-cost retina procedures, and level 3 (APC 5493), which includes higher-cost and/or more resource intensive procedures, will be increased by more than the 3.3% average (Table 1).
“We are grateful that intraocular levels 2 and 3 received higher than the average increase of 3.3% (4.97% and 5.69%, respectively) and CMS specifically acknowledged our concerns with their plans to monitor payment adequacy of retinal detachment procedures,” said Geoffrey G. Emerson, MD, PhD, FASRS, president of the American Society of Retina Specialists (ASRS), which was among several ophthalmology organizations lobbying for the increase. “We, however, remain concerned about the flawed APC methodology, which by design creates winners and losers.”
Dr. Emerson explained that CMS determines APC payments by totaling the costs for every procedure in the category, then determining the geometric mean. This approach enables Medicare to set a “typical” payment that isn’t skewed by a few very high-cost (or low-cost) procedures. However, the APC methodology creates disparities, with complex retinal surgeries often underpaid relative to their true practice costs. “Instead of calculating the practice expense for each CPT code, as is done for the Medicare Physician Fee Schedule, OPPS lumps similar procedures together in APCs and pays all procedures in the category the geometric mean,” he explained. “For example, intraocular level 2 has 33 procedures with costs ranging from $859 to $5312.33, with an OPPS payment of $4222.95. Because the average weighted cost of retinal detachment surgery (CPT 67108) is $4,818.85, every procedure loses $595.90.”
Another concern for ASRS, as well as organizations like the American Academy of Ophthalmology (AAO) and the Outpatient Ophthalmic Surgery Society (OOSS), involves access to emergency retina care under OPPS. In ASRS’s most recent Preferences and Trends survey, 71% of retina specialists reported difficulty securing adequate operating room time for emergency cases such as retinal detachment repair. A letter to CMS during the comment period noted that surgical block time at ASCs has often been reduced or eliminated because reimbursement for retinal detachment and other procedures fail to cover the actual costs, resulting in significant financial losses. The comment emphasized that these restrictions often shift cases to higher-cost settings, which runs counter to CMS’s stated goal of providing care in the most cost-effective environment.
“Making the OR access situation even worse is the fact that many retinal detachment surgeries present after hours or on the weekend, and ASC’s do not want to extend their normal hours and pay additional staff costs to accommodate emergency surgeries that are already in the red,” said Dr. Emerson. “We look forward to working with CMS on a solution that will ensure Medicare patients have timely access to sight-saving emergency retina procedures.”
According to CMS, these payment policies affect approximately 4,000 hospitals and approximately 6,000 ASCs. RP