A research project involving more than 1,000 retinal detachments offers a glimpse into how artificial intelligence (AI) might one day assist physicians with complex diagnostic decisions. In this project, an AI model was able to match—and in many cases, exceed—the performance of Lincoff’s well-known rules for predicting the location of retinal breaks.
For John T. Thompson, MD, who presented “Lincoff vs Artificial Intelligence: A Reappraisal of Lincoff's Rules for Finding the Retinal Tear” on Thursday at the American Society of Retina Specialists (ASRS) annual meeting in Long Beach, California, the AI model’s accuracy was impressive. However, the most important takeaway, he said, was how the exercise demonstrates what AI can do when trained on real-world clinical data. “This is a great example of how AI can look at patterns in large data sets and extract insights that even experienced clinicians might miss,” observed Dr. Thompson.
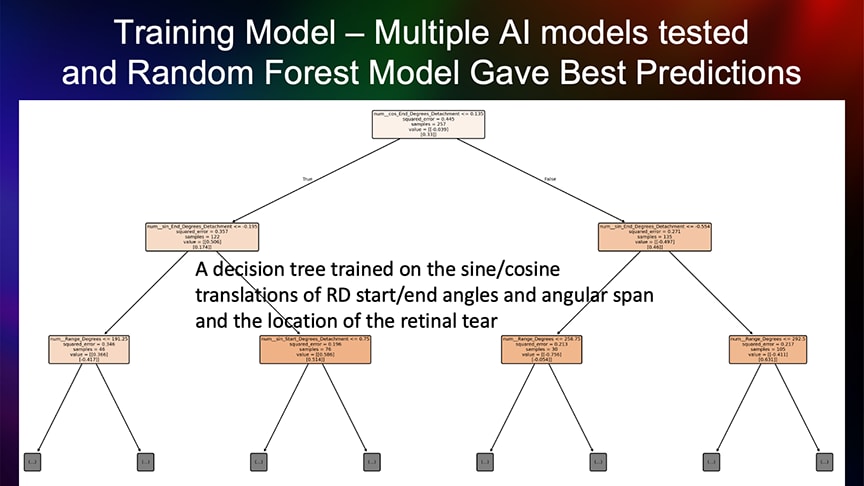
Figure 1. A random forest model was trained on data from 1,031 retinal detachment cases to predict detachment patterns based on eye laterality, break position, and detachment location.
Lincoff’s rules, developed during the 1970s by the late Harvey Lincoff, MD, are a set of 4 heuristic guidelines used to infer the location of a retinal tear based on the configuration of the detachment—for example, superior detachments ending at the horizontal meridian are usually caused by a break at the highest point of the detachment. Lincoff’s rules are commonly taught in fellowship programs and remain a mainstay in situations where a break cannot be directly visualized.
To test the predictive power of these rules, Thompson enlisted Viviana Lee, an undergraduate at Johns Hopkins University, who developed the predictive modeling using AI. “Viviana deserves the credit for the modeling and analysis,” he said. “She’s the brains behind this AI project.”
Using data from Dr. Thompson’s charts for 1,031 patients with rhegmatogenous retinal detachment, Lee constructed a data set that included the extent and clock-hour location of every detachment, whether it occurred in a right eye or left eye, and the position of all retinal breaks. Eighty percent of the data set was used to train a random forest model—a type of machine learning algorithm that builds multiple decision trees and combines their outputs to improve prediction accuracy (Figure 1). The remaining 20% of the data set was reserved to validate the model’s predictive performance.
“The data we provided to the model was: here is a detachment from 12:00 to 4:00 in a right eye—now where is the tear most likely to be?” explained Dr. Thompson. “The model wasn’t told about Lincoff’s rules; it was trained entirely on actual tear locations from my patient population.”
For eyes with a single tear, the AI model made more accurate predictions than Lincoff’s rules 95% of the time. Accuracy was similar for eyes with 2 tears (94.5%) and 3 tears (96.4%). “That tells us the model isn’t just memorizing patterns—it’s identifying underlying rules based on the data,” Dr. Thompson said. “That’s what Lincoff did by hand, with a similar number of cases as our study.”
Dr. Thompson framed the project as a broader demonstration of how AI can be used in clinical ophthalmology—not to replace clinicians, but to support their work with data-driven guidance. “This shows what’s possible,” he said. “We already have FDA-approved AI tools that can screen for diabetic retinopathy. There’s no reason we can’t build similar tools for predicting tear location, surgical planning, or postoperative management. That’s the kind of AI I think we need more of in medicine.” RP